ECZEMAPEDIA
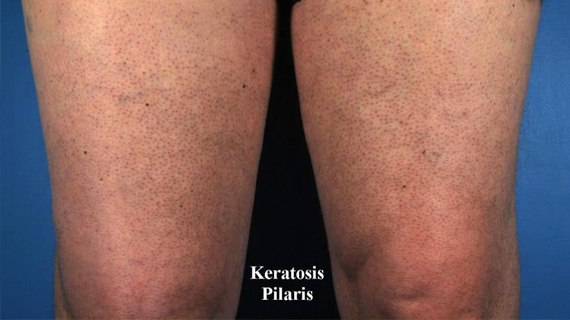
KERATOSIS PILARIS (“CHICKEN SKIN”)
Keratosis pilaris (KP) yang juga dikenali sebagai “chicken skin” merupakan keadaan kulit yg lazim berlaku. Biji-biji yang kelihatan seperti jerawat ini sebenarnya adalah sel kulit yang mati yang menyumbat folikel rambut. Jerawat ini boleh berwarna merah atau perang. Ia biasanya wujud di bhg atas lengan, peha, pipi atau punggung. Ia tidak berjangkit dan biasanya tidak gatal dan tidak menyebabkan sebarang masalah. KP boleh bertambah teruk apabila cuaca kering dan bila kulit kering. Ia juga boleh bertambah teruk semasa mengandung.
KP adalah penyakit kulit yang ada kaitan genetik dan tidak mempunyai rawatan tertentu . Ia biasanya akan hilang secara sendiri bila seseorang mencapai umur 30an.
SYMPTOM KP
Simptom utama KP adalah biji biji yang timbul yang menyerupai seperti kulit ayam yg telah dicabut bulunya. Ia boleh timbul di mana folikel rambut wujud. Oleh itu, KP tidak akan timbul di kawasan tapak tangan dan tapak kaki. Ia lebih kerap berlaku di bhg atas lengan dan peha. Ia boleh juga timbul di bhg kaki dan tangan yang lain. Simptom yang lain adalah:
-
- warna merah sekeliling biji tersebut
- Kulit yang rasa gatal
- Kulit yang kering
- Biji biji yang timbul yang rasa seperti kertas pasir
- Biji tersebut boleh mempunyai warna yg berbeza bergantung pada warna kulit (putih, merah, merah jambu, hitam atau perang)
PENYEBAB KP
Keadaan kulit yang benign ini adalah disebabkan oleh pengumpulan keratin iaitu sejenis protein rambut di dalam liang roma. Jika anda mempunyai KP, ini bermakna keratin rambut anda telah menyumbat liang pori rambut. Akibatnya, biji biji kecil yang timbul wujud di bhg di mana rambut sepatutnya wujud. Jika anda menggaru biji tersebut, anda mungkin dapat melihat rambut yang hauls di bhg bawah biji tersebut.
Penyebab pengumpulan keratin ini masih tidak diketahui, tapi ada pakar yang berpendapat ianya ada kaitan dengan penyakit kulit yg lain seperti atopic dermatitis (eksema) dan penyakit genetik yg lain.
SIAPA YANG BOLEH MENDAPAT KP?
Ia lazim berlaku pada mereka yang mempunyai:
-
- kulit kering
- Eksema
- Ichytosis
- Resdung
- Melanoma
- Obese
- Wanita
- Kanak-kanak atau remaja
KP lebih kerap berlaku pada kanak-kanak dan remaja dan biasanya akan hilang semaa pertengahan umur 20an dan dalam kebanyakan kes, hilang sepenuhnya semasa umur 30an. Perubahan hormon semasa mengandung atau semasa mencapai baligh boleh menyebabkan KP bertambah teruk. KP lebih lazim berlaku pada mereka yang mempunyai kulit yg cerah.
CARA RAWATAN
Tidak ada ubat yg boleh menyembuhkan KP dan biasanya tidak banyak rawatan yang boleh membaiki keadaannya. Antara teknik yang boleh dipakai adalah:
-
- Memakai pelembap untuk mengelakkan kulit menjadi kering. Pelembap yang mengandungi urea dan asid laktik adalah sesuai utk mengeluarkan sel kulit yg mati dan menghalang folikel rambut dari tersumbat.
- Microdermabrasion
- Chemical peels
- Krim retinol
Ramuan dalam krim diatas boleh menyebabkan iritasi dan rasa pedih dan boleh mengeringkan kulit, oleh itu, ia mestilh dipakai selepas mendapat nasihat pakar kulit.
RAWATAN RUMAH
Anda juga boleh mencuba teknik-teknik ini di rumah spt:
-
- Mandian dengan air suam untuk jangka pendek untuk melembutkan liang pori yg tersumbat dan berus dengan berus lembut di bhg biji tersebut. Proses ini mesti dilakukan utk jangka pendek kerana ia boleh mengeringkan kulit juga.
- “Exfoliation” (pengeluaran sel kulit mati) boleh dilakukan dengan kerap menggunakan loofah atau batu pumis.
- Mengguna kan minyak kelapa sebagai bes untuk sugar scrub untuk mengeluarkan sel kulit mati dan meredakan kulit yg merah dan radang.
- Elak dari memakai pakaian yg ketat
- Guna humidifier di rumah supaya udara di bilik tidak kering